The Healthcare Industry Has A Talent Crisis: We Found The Cure.
We just completed a massive study of the talent and HR challenges in healthcare, and the findings are astounding. And there is a lot to learn from this industry.
To start, you should understand that healthcare is now the largest industry in the United States. Almost 14% of the American workforce serves in this industry, representing almost one in seven American workers. These individuals play many roles, but over 80% are directly involved in the delivery of care.
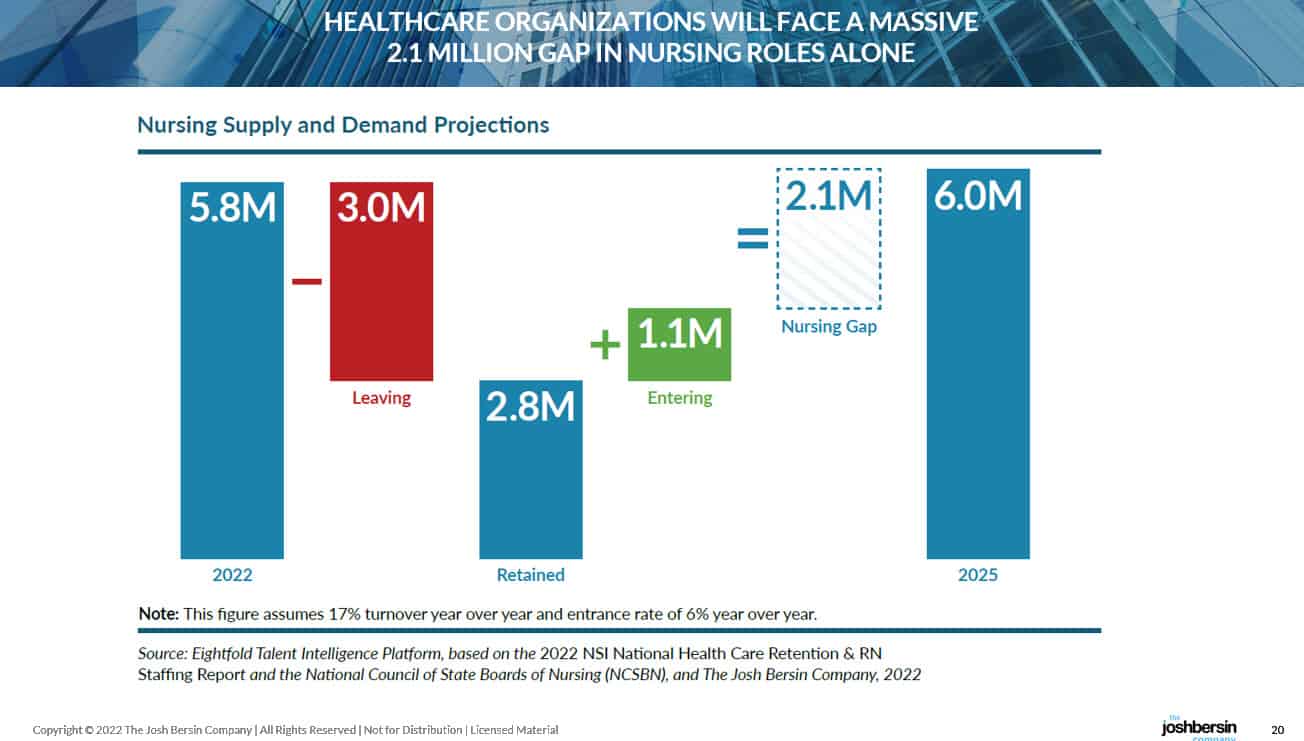
Using the massive workforce database of Eightfold.ai, we analyzed these 20+ million workers and found that they fall into six major job clusters (Eightfold AI is a large time-series based, AI-powered database of workers around the world). Among these clusters, the largest and most stressed are nurses. There are about 5.8 million nursing professionals in the US (almost 750,000 are open at any time), and these individuals make up the foundational roles in our healthcare.
Nurses are not only people who wear white hats and give you injections: they help people with trauma, the assist physicians, they dispense medicine, and they counsel and heal us when we’re sick. These are the people who saved us during the pandemic.
Hospitals, clinics, and providers know quite well that nurses are their biggest talent challenge. Not only are these important people, they are highly trained, they work very hard, and many of them have children, family responsibilities, and complex work arrangements with their employer. So the industry has become very creative at finding ways to recruit, hire, employ, train, and retain nurses.
That all said, the industry has some problems. Many hospitals admit to us that their nurse (caregiver) turnover can be as high as 60% or more, and the Glassdoor ratings show hundreds of comments about overwork, toxic work environment, and all sorts of poor working conditions. One CHRO told me that “our nurses are going through more trauma than our patients,” and I can understand why. (A new study on caregiver mental health just found that 83% of nurses feel anxiety, 81% are exhausted and 77% feel overwhelmed. )
These workers report regularly feeling stress (91%), anxiety (83%), exhaustion/burnout (81%) and overwhelmed (77%). In the last three months, 3/4 report an increase in physical exhaustion and having trouble falling asleep, half experienced an increase in headaches, stomachaches and change in appetite, more than one-third experienced an increase in racing thoughts and roughly one-fourth reported an increase in likelihood to smoke, drink or use substances.
Many Providers, Wide Variations In Management Expertise
Healthcare delivery is a big and diverse industry. There are more than 6,000 different hospitals, networks, and clinics in the US, each managed by a different leader. When you look at Glassdoor ratings among hundreds of providers you find a huge range of ratings: the lowest rated provider has an aggregate rating of 2.4 (very low) and the highest (a research hospital) is 4.3, as high as Microsoft or Google.
Press Ganey, the organization that specializes in employee and patient feedback, actually found that in Q2 of this year, on average, two nurses were assaulted every hour. Taking care of nurses is not only a problem for HR: patients abuse nurses so there must be security and reporting practices in place.
What this means, of course, is that Employee Experience in nursing is very complex. Imagine running a business with facilities, mission-critical technology, transportation staff, and all the traditional functions of finance, HR, and legal – in addition to a large workforce doing life or death care, often dealing with unstable patients. The complexity of roles and skills in healthcare is an order of magnitude more complex than most other businesses. And that’s why we studied it in detail.
What did we discover?
Let me summarize the research with a couple of important findings, and I think you’ll find them fascinating and educational for your own company.
First, there is going to be a massive gap in talent, skills, and people. Our research, which used time-series analysis, retention data, and lots of economic data, shows that the US healthcare industry will be short 2.1 million nursing professionals over the next three years. This is a very big number – dwarfing jobs like software, data science, and cyber security.
 |
Second, the industry is not well prepared to find these people.
During the process of conducting this research, we developed a model we call the “Four R’s” – Recruit, Retain, Reskill, and Redesign. These four talent practices must fit together to deal with any talent challenge, and in healthcare they point out some significant opportunities.
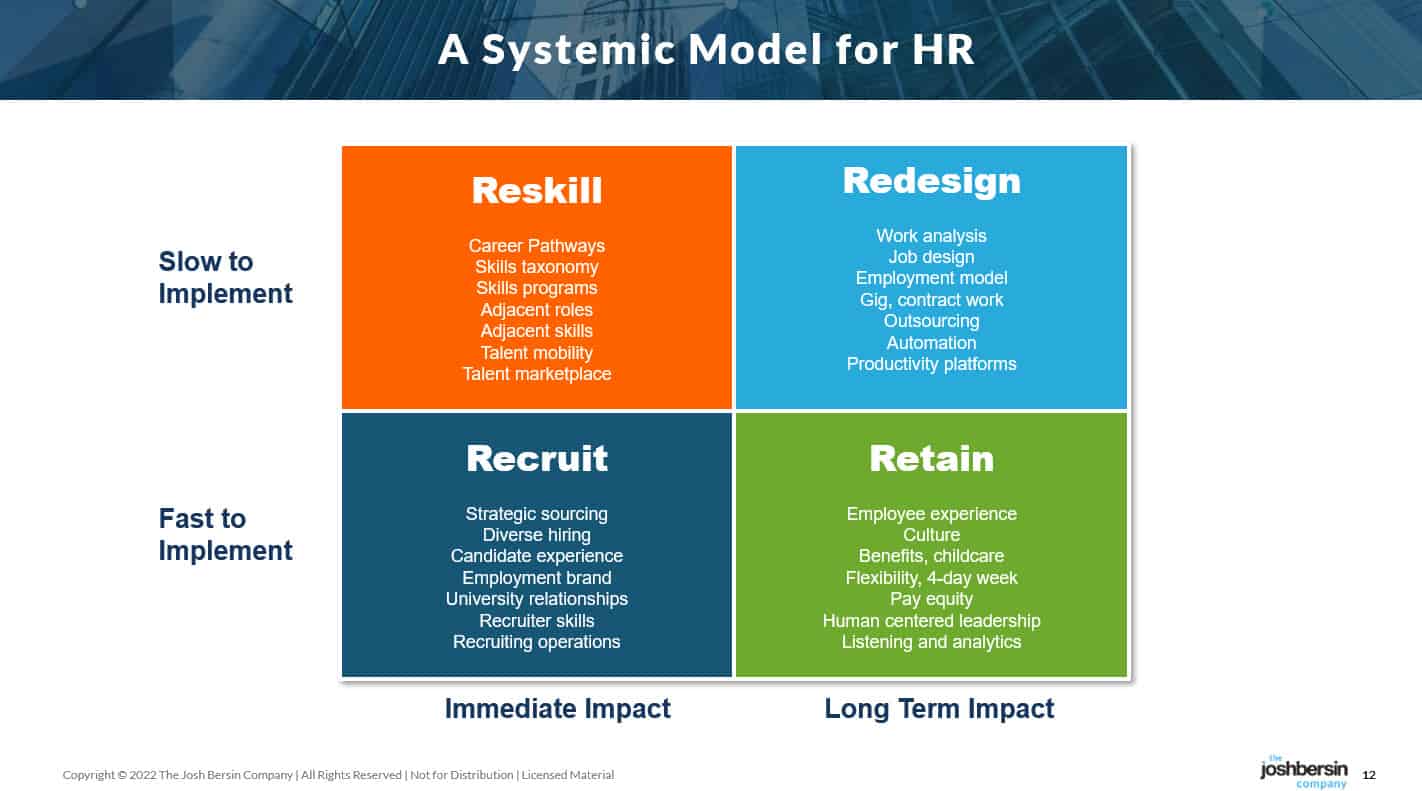 |
If you look at the total number of registered nurses and those graduating from nursing school each year, this industry can only Recruit around 350,000 nurses over the next three years. Retention, which is a big and difficult effort, (often involving a heavy focus on employee experience, work arrangements, pay, and more), can preserve as many as 400,000. But this is limited: the average age of a nurse is 52, so many will simply retire or decide to work part-time.
Reskilling, which we all think is exciting, is slow and time consuming. Many companies are doing amazing things to reskill and build new career pathways in healthcare, but it takes years to deliver impact. Our research shows that approximately 500,000 nursing professionals can be developed this way, and that includes programs like Amazon’s Career Choices program that teaches hourly logistics workers to transition into healthcare.
That leaves us with a big gap: around 850,000 jobs simply cannot be filled. What can we do?
This gets us to one of our biggest findings: the need to Redesign jobs, roles, work arrangements, and operations in healthcare. We just finished a major study of organization design this year and this fourth R is now urgent throughout this industry.
Working At The Top Of Your License
As we talked with healthcare leaders, we constantly heard about the need for nurses to operate at “the top of their license.” This concept, which we believe is instrumental in every major role in business, means that nurses should do nursing. They shouldn’t waste time on record-keeping, cleaning rooms, searching for medications, or wasting time scheduling others. Many CHROs told us that most nurses spend at most 30% of their time doing nursing, which implies that we could more than double our capacity if we designed care differently.
Staffing at top-of-license means physicians and clinicians practice to the highest extent of their education, training, and experience. For example, an RN would focus on complex patient care while a clinician with less training and education (who would also be less expensive) would take a basic patient-facing role.
Greg Till, the CHRO of Providence, has put in place a program to decompose the clinical care problem, and assign accountability to each element to the “right person” or the “right platform.” Through this design work, coupled with an AI-based scheduling system and other automation and augmentation, they have saved nurses thousands and thousands of hours. We all need to learn how to do this, and our org design research shows you the way.
Our study found that around 850,000 “job equivalents” must be removed from this talent demand, leading the healthcare industry into a big world of job redesign, new roles, and automation. This is not “robotic automation” at all, by the way. It’s a focus on carefully designing the patient experience and making sure the right roles are designed to optimize every stage.
We dove into this topic, and found that among the hundreds of companies we studied, around 15% are “really good” at optimizing their care delivery systems. (The others are suffering from terribly low Glassdoor ratings, burned out workers, and a never-ending need to hire.) These companies, the ones we call the “advanced healthcare organizations”, have significantly different skills and roles in their companies. They have comprehensive tech, transformation, and change capabilities – skills that hardly feel like healthcare at their core.
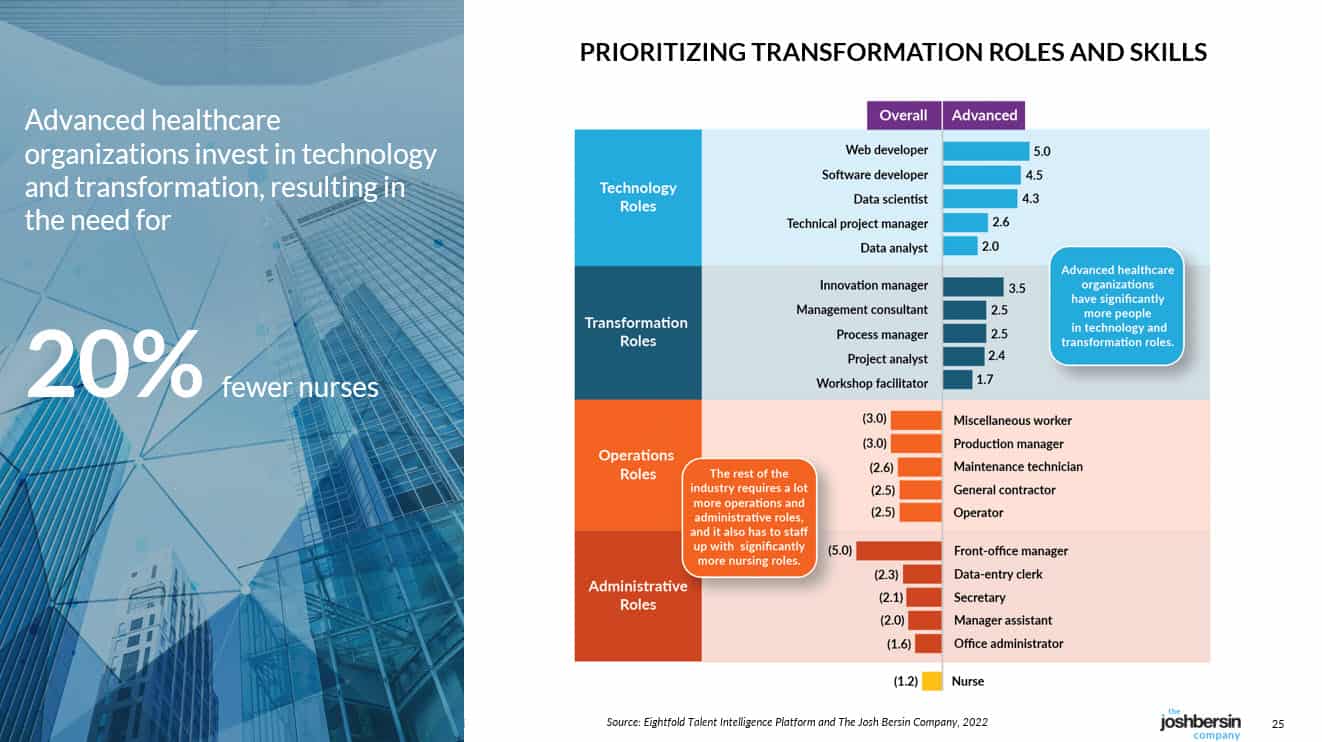 |
What’s The Lesson To You?
I was asked by a reporter: “do you think the healthcare industry will adapt?” My answer is this: many providers will adapt, some will be acquired, and others will be disrupted.
Consider the way others are entering the space. Amazon just acquired OneMedical, CVS acquired Signify Health, Walmart introduced Walmart Health, and Walgreens Boots acquired CareCentrix. Last week Telus acquired Lifeworks, and we can expect more to come. These deals are all examples of what we call “Industry Transformation,” companies with strong business models leveraging their strength to expand. The pressure on healthcare providers will just grow.
The lesson from this research applies to nearly every industry. If you’re not transforming your jobs, employment model, employee experience, and benefits all at once, you cannot “hire your way out” of this challenge. Healthcare, like every other industry, is being disrupted by growth, change, technology, and competition. Designing your company to be Irresistible is the only solution you have.
(Read the WSJ article about how Starbucks is now redesigning its entire operating model to meet their hiring and talent challenges.)
Healthcare is an industry filled with committed care professionals. In the future it will be their strategic thinking, organization design, technology, and transformation skills that matter.
Isn’t that a lesson for all of us?
Stay tuned for more – the research is fascinating, and you can join our corporate membership to learn more.
Additional Resources
Healthcare At A Crossroads: Research Details
The Global Workforce Intelligence Project